|
E-Mail Edition Volume 12 Number 2 |
|||
|
Published Spring, 2015 Published by Piccadilly Books, Ltd., www.piccadillybooks.com. Bruce Fife, N.D., Publisher, www.coconutresearchcenter.org
|
|
||
|
If you would like to subscribe to the Healthy Ways Newsletter |
Contents
|
||
|
|
The U.S. Government to Withdraw Longstanding Warnings About Cholesterol
"Cholesterol is no longer considered a nutrient of concern for overconsumption," reports the US Department of Health... Have you restricted your consumption of eggs,
meats, and dairy in fear that they might raise your blood cholesterol
levels? If so, you no longer need to worry. After years of debate about
the perceived dangers of consuming cholesterol, the nation's top nutrition
advisory panel has decided to drop its caution about eating cholesterol-laden
food, a move that could undo almost 40 years of government warnings
about its consumption. Every five years, the United States Department
of Health and Human Services updates a set of Dietary Guidelines
intended to help Americans make healthier food choices. These guidelines
also help establish regulations and standards food companies follow
in labeling their products. The 2015 edition will mark perhaps the biggest
change since the original 1977 Guidelines by dropping the warning about
cholesterol consumption. One of the six core goals since the 1970s has
been to limit the intake of cholesterol to less than 300mg per day,
however the present Dietary Guidelines Advisory Committee (DGAC) believes
that cholesterol consumption is no longer something we need to worry
about. The group's decision follows an evolution of
thinking among many nutritionists who now believe that eating foods
high in cholesterol may not significantly affect the level of cholesterol
in the blood or increase the risk of heart disease. Blood cholesterol
level is carefully regulated and is not haphazardly influenced by diet.
This is why dietary approaches can alter blood cholesterol by less than
10 percent. The amount of cholesterol produced within our bodies every
day is much larger than what we get from our diet. Therefore, the amount
we consume has no significant bearing on blood cholesterol levels. Foods high in cholesterol — such as eggs, red
meat, and seafood — have long been considered contributors to the risk
of heart disease. Years of research seeking to establish a possible
causative link between them and undesirable health outcomes has been
a failure. In the absence of a proper scientific consensus and given
that the human body produces a lot more cholesterol than it takes in
via the diet, the DGAC has decided that "cholesterol is not considered
a nutrient of concern for overconsumption." Therefore, the amount of
it that you consume is no longer thought to be important enough to restrict. While Americans may be accustomed to conflicting
dietary advice, the change on cholesterol comes from the influential
Dietary Guidelines Advisory Committee, the group that provides the scientific
basis for the "Dietary Guidelines." That federal publication has broad
effects on the American diet, helping to determine the content of school
lunches, affecting how food manufacturers advertise their wares, and
serving as the foundation for dietary advice given by doctors and government
agencies. Many nutritionists said lifting the cholesterol
warning is long overdue, noting that the United States is out-of-step
with many other countries, where diet guidelines do not single out cholesterol. "There's been a shift of thinking," said Walter
Willett, MD, chair of the nutrition department at the Harvard School
of Public Health. He called the turnaround on cholesterol a
"reasonable move." But the change on dietary cholesterol also shows
how the complexity of nutrition science and the lack of definitive research
can contribute to confusion for Americans who, while seeking guidance
on what to eat, often find themselves afloat in conflicting advice. Cholesterol has been a fixture in dietary warnings
in the United States at least since 1961, when it appeared in guidelines
developed by the American Heart Association. Later adopted by the federal
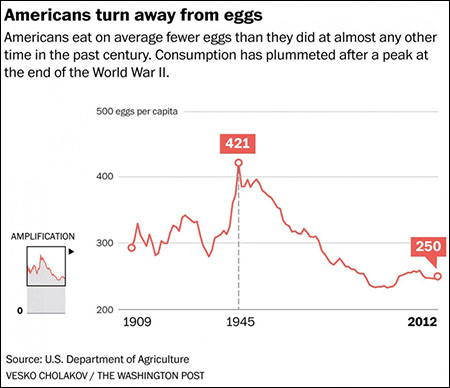
government, such warnings helped shift eating habits and dropped egg
consumption by 30 percent.
Even as contrary evidence has emerged over the
years, the campaign against dietary cholesterol has continued. In 1994,
food-makers were required to report cholesterol values on nutrition
labels. In 2010, with the publication of the previous "Dietary
Guidelines," the experts again focused on the problem of "excess
dietary cholesterol." Yet many have viewed the evidence against cholesterol
as weak, at best. As late as 2013, a task force arranged by the American
College of Cardiology and the American Heart Association looked at the
dietary cholesterol studies. The group found that there was "insufficient
evidence" to make a recommendation. Many of the studies that had been
done, the task force said, were too broad to single out cholesterol. "Looking back at the literature, we just couldn't
see the kind of science that would support dietary restrictions," said
Robert Eckel, the co-chair of the task force and a medical professor
at the University of Colorado. The previous guidelines called for restricting
cholesterol intake to 300 milligrams daily. (For comparison, the yolk
of a single egg has about 200 milligrams.) American adult men on average
ingest about 340 milligrams of cholesterol a day, according to federal
figures. That recommended figure of 300 milligrams, Eckel said, is
"just one of those things that gets carried forward and carried
forward even though the evidence is minimal." Other major studies have indicated that eating
one or two eggs a day does not raise a person's risk of heart disease. While reversals in dietary recommendations might
seem aggravating, it is a sign of progress. "These reversals in the
field do make us wonder and scratch our heads," said David Allison,
a public health professor at the University of Alabama at Birmingham.
"But in science, change is normal and expected." When our view of the cosmos shifted from Ptolemy to
Copernicus to Newton and Einstein, Allison said, "the reaction was
not to say, 'Oh my gosh, something is wrong with physics!' We say,
'Oh my gosh, isn't this cool?' " Allison said the problem in nutrition stems
from the arrogance that sometimes accompanies dietary advice. Because
a scientific body comes to a consensus about a particular issue, some
people take this as the absolute final word on the subject and ignore
contradictory evidence and ridicule those who question the status quo.
Now all those who have shouted the warning about eating cholesterol
and criticized those who questioned this advice have egg on their face.
A little humility could go a long way. Despite the change in position about dietary
cholesterol, many people are holding on to cherished opinions that fat
and cholesterol are bad and continue to shout warnings about eating
saturated fat and the dangers of high blood cholesterol. These people
are soon to find egg on their face as well. In recent years two major meta-analysis studies
which combined all previous studies on saturated fat and diet showed
that those people who eat the most saturated fat have no more incidence
of heart disease than those who eat the least, proving that saturated
fat does not cause or promote heart disease. A new meta-analysis study published February
2015 reexamined all of the data available in 1977, when the Dietary
Guidelines were first issued, concluded that the original recommendations
were based on inadequate evidence and should never have been issued.
The report, authored by an international team of researchers, was critical
of the advice against the restriction of dietary saturated fat, which
could, with time, be another area where the DGAC seeks to modify its
recommendations. The researchers concluded that a correlation
between saturated fat consumption and coronary heart disease was just
a hypothesis without good supporting evidence when the US government
issued its Guidelines in 1977 and echoed by the UK and other countries
soon thereafter.
The dietary recommendations focused on reducing dietary fat intake;
specifically to (1) reduce overall fat consumption to 30 percent of
total energy intake and (2) reduce saturated fat consumption to 10 percent
of total energy intake. Later the recommendation for saturated fat was
reduced further to 7 percent. Dr. Zoe Harcombe of the University of the West
of Scotland and lead author of the study, stated that these recommendations
"were untested in any trial prior to being introduced," As there is
today, when these guidelines were issued there was no evidence that
eating less fat or saturated fat would improve a person's heart health.. Among the data on dietary fat consumption and
heart disease that was available at the time, there were no differences
in the number of deaths from all causes, and no statistically significant
changes in death from cardiovascular disease. Eating less saturated
fat was not shown to improve a person's heart health, even where changes
in diet led to a reduction in blood cholesterol levels. "It seems incomprehensible
that dietary advice was introduced for 220 million Americans and 56
million UK citizens, given the contrary results from a small number
of unhealthy men," says Harcombe. At the time of issuing the original 1977 Dietary
Guidelines for the United States, the committee's lead nutritionist,
Dr. Hegsted of Harvard University, admitted that the evidence base for
the restriction on saturated fat was lacking. "There will undoubtedly
be many people who will say we have not...demonstrated that the dietary
modifications we recommend will yield the dividend expected," remarked
Hegsted. But his counterargument was that there was more to gain from
switching to the recommended diet than there was to lose. Such a statement
was based more on wishful thinking than good science. The longstanding advice to increase the consumption
of carbohydrates as a way to offset the reduction in total fat and saturated
fat may now be proving Dr. Hegsted's assertion wrong as subsequent research
has now shown that
low-carbohydrate diets are more effective at promoting better health
than low-fat ones. The conclusion of the Harcombe study is clear
and to the point: "The present review concludes that dietary advice
not merely needs review; it should not have been introduced." It's remarkable
that national and international dietary guidelines, that affect the
health of millions of people, have and are being issued and vigorously
supported and defended without proper scientific evidence. In fact,
a great deal of weight in the argument against the consumption of saturated
fat has been based on the Dietary Guidelines. Anti-saturated fat proponents
have used the Dietary Guidelines as proof that saturated fat is unhealthy
and trumps all the studies that claim differently. After all, a scientific
committee representing a government body must be correct—right? Several years ago I wrote a detailed overview
on coconut oil and submitted it to Wikipedia. I included an extensive
section on the health aspects of coconut oil and meticulously backed
every statement with references to published medical studies. They posted
the article but within days most of the article was replaced, including
all of the health section. In its place was a brief statement that coconut
oil is just another saturated fat and should not be consumed, as proof
the article referenced the Dietary Guidelines of the United States and
several other countries and organizations who have copied these same
guidelines. While other parts of the coconut oil article on Wikipedia
have changed over the years, this health section has remained the same. Sources:
http://www.health.gov/dietaryguidelines/2010.asp. Whoriskey,
Peter. The U.S. government is poised to withdraw longstanding warnings
about cholesterol. The Washington Post February 10, 2015.
Harcombe,
Z, et al. Evidence from randomized controlled trials did not support
the introduction
of
dietary fat guidelines in 1977 and 1983:
a systematic review and meta-analysis. Open Heart 2015;
doi:10.1136/openhrt-2014-000196. Chowdhury, R., et al. Association of dietary,
circulating, and supplement fatty acids with coronary risk: a systematic
review and meta-analysis. Ann Intern Med 2014;160:398-406. Siri-Tarino, PW, et al. Meta-analysis of prospective
cohort studies evaluating the association of saturated fat with cardiovascular
disease. Am J Clin Nutr 2010;91:535-546.
|
||
|
|
|||
 |
Drink for Your Health?
Don't Bet Your Life on It
Alcohol
may not be so healthy after all. New study exposes flaw in previous
studies. Benefits of alcohol consumption questioned. A number of studies in recent years have suggested
that moderate alcohol consumption may help reduce the risk of heart
disease and death. The idea that alcohol consumption might be good for
our health has inspired hope among drinkers. But a new study by a group
of British and Australian researchers largely squashes that hope.1
According to this new study, unless you're a woman over the age of 65,
alcohol consumption is unlikely to forestall your death. And for these
older women, the health benefits of alcohol are small. Like several previous studies, this new study
initially returned findings indicating that men between the ages of
50 and 65 might reap a small benefit from drinking 1 to 2 glasses of
alcohol a day. But those apparent benefits completely evaporated when
the researchers removed from their nondrinking "reference group" all
those people who used to drink but had stopped. |
||
|
This strange twist does more than disappoint
middle-aged men eager to believe that alcohol makes them more robust.
It also casts doubt on all the previous studies that have concluded
that modest drinkers are healthier than nondrinkers (or never drinkers). It turns out that former drinkers exhibit poorer
health and have a higher risk of death, many of whom quit drinking due
to ill health or are recovering alcoholics. Former drinkers are a much
less-healthy group than people who simply never drink at all. But researchers
often lump these former drinkers together with people who have always
been teetotalers (never drinkers). The authors of the current study
estimate that more than half of those who call themselves nondrinkers
are misclassified as never drinkers. |
 |
||
|
The inclusion of these less-healthy former drinkers
makes the average health of "nondrinkers" look poorer. In comparison,
those who consume alcohol tend to look healthier. In the current study, when these former drinkers
were expunged from the comparison-group of teetotalers, the nondrinking
group suddenly looked healthier. And the bar for showing alcohol's health
benefits rose. The apparent benefits of alcohol vanished. This study suggests that the many previous studies
finding health benefits associated with alcohol consumption suffer from
the same fatal flaw. The benefits of alcohol consumption, therefore,
have generally been overstated in recent research. This is not the first study to identify this
fatal flaw in alcohol studies. An earlier meta-analysis study that reexamined
54 previous studies found that the removal of former drinkers from the
nondrinkers categories resulted in an attenuation or complete nullification
of the reported protective effects.2 This study pretty much
nullified the conclusions all of the previous studies showing benefits
to alcohol consumption. Another possible problem with previous studies
is "selective bias" of the participants. The small benefit seen in women
over 65 in this current study, even after removing former drinkers,
may have been due to this. Only apparently healthy participants free
of prevalent disease at the time of enrolment were included in these
studies. The protective effects commonly identified among the studies
may occur partly as a function of selection biases—tthe selection of
healthy participants. If so, rather than moderate alcohol consumption
being directly involved in the attenuation of mortality risk, it may
simply represent an unidentified lifestyle trait specific to healthier
people. References
1. Knott, CS, et al. All cause mortality and
the case for age specific alcohol consumption guidelines: pooled analyses
of up to 10 population based cohorts. BMJ 2015;350:h384. 2. Fillmore, KM, et al. Moderate alcohol use
and reduced mortality risk: systematic error in prospective studies
and hypotheses. Ann Epidemiol 2007;17(5 Suppl):S16-23.
|
|||
|
|
|||
|
Do you have friends who would like this newsletter? If so, please feel free to share this newsletter with them.
If this newsletter was forwarded to you by a friend and you would like to subscribe, click here.
Copyright © 2015, Bruce Fife. All rights reserved.
|
|||