

Dietary fat, and saturated fat in particular, is essential for good health. Not only does it provide the basic building blocks for cells, tissues, and hormones, but is essential for establishing a healthy gut microbiome and an effective immune function. read more
New research has shown that the MCFAs in coconut oil can kill Enterococcus faecalis, a disease-causing bacterium that is responsible for as much as 80 percent of all human infections. read more
Canola oil is one of the most commonly used foods in food processing and restaurants. A new study suggests that frequent consumption of canola oil can lead to brain damage and memory loss. read more
According to a new study published in the journal Neurology, lowering LDL cholesterol too much can increase the risk of stroke. read more
Superfoods are known for their extraordinary health and healing properties. Among all the superfoods, there is one that stands head and shoulders above the rest. read more
Issue 16-3 covers: Does Low Cholesterol Cause Alzheimer’s? —Keto Cycling: How to Optimize the Ketogenic Diet and Avoid Common Mistakes— Consumer Alert! Do You Know Where Your Foods and Supplements Come From? —Why Scientists Are Opposing 5G Networks. read more
Mother’s Milk Protects Infants from Infection
We live in a sea of microorganisms; they are in the air we breathe, the food we eat, the water we drink, and even live on our bodies. Some of these microbes are relatively harmless and can even be beneficial, while others can cause sickness and death. For the most part, our immune system protects us from infection from the more malevolent varieties.
When an infant is born, it comes from the relatively sterile environment of the womb into a world that is teeming with potentially harmful germs. At this stage of life the immune system is not fully developed and the infant is highly vulnerable to infection. Fortunately, infants are not born defenseless; mother’s milk contains several substances that protect infants from infections during this critical time. Some protection comes from the mother’s antibodies in her milk, but perhaps the greatest protection comes from its fat content.
Mother’s milk is rich in fats, mostly saturated and monounsaturated fats, with some polyunsaturated fat to supply the infant’s essential fatty acid needs. These fats serve multiple functions; they provide nourishment, help to establish a healthy gut microbiome, and ward off infection and disease.
Long chain fatty acids (LCFAs) from our foods modulate intestinal immune function, which is independent of the systemic immune system. The absorption of LCFAs stimulates the influx of lymphocytes, a type of white blood cell, through the intestinal wall. This process helps defend against potentially harmful microorganisms that may have found entry into the gastrointestinal tract from the meal.[1] Germs can be carried into the body by any type of food—milk, vegetables, fruits, grains, and so forth. Including some fat with meals helps protect against infection. Mother’s milk naturally supplies the fat necessary to do this.
Fatty Acids Kill Disease-Causing Microorganisms
In addition, many fatty acids, especially those in breast milk, possess potent antimicrobial properties capable of killing troublesome bacteria, viruses, fungi, and parasites. These fatty acids are powerful enough to kill intestinal troublemakers like E. coli, H. pylori, and Candida albicans, yet completely harmless to human cells. Unlike antibiotics that kill all bacteria, fatty acids are more selective; they can kill the major troublemakers yet leave the good bacteria alone. In this way, potential troublemakers are suppressed while the good microbes are allowed to thrive and firmly establish themselves in the infant’s digestive tract, producing a healthy gut microbiome.
The fats we eat are composed of triglycerides. Triglycerides consist of three fatty acids joined together by a glycerol molecule. When fats are consumed and digested, the triglycerides are gradually broken down into diglycerides (two fatty acids joined by a glycerol), monoglycerides (one fatty acid attached to a glycerol), and individual fatty acids. It is the monoglycerides and fatty acids that have the antimicrobial properties. Triglycerides and diglycerides have none.
Some fatty acids are more effective at killing certain types of microorganisms than others. Some kill bacteria like E. coli, others kill streptococcus and staphylococcus, and still others yeasts and viruses. For example, capric acid, a 10 chain saturated fatty acid, is more effective at killing certain bacteria than caprylic acid, an 8 chain saturated fatty acid; however, caprylic acid is more effective at killing certain fungi than capric acid. Natural fats contain a mixture of several different types of fatty acids, so they are effective against a wide variety of pathogens.
Fats Boost Immune Function
The antimicrobial effect varies greatly among the different fatty acids. Some are very potent while others are rather weak. Some LCFAs that are common in our everyday foods, such as oleic and linoleic acids, possesses some antimicrobial effects. However, medium chain fatty acids (capric, caprylic, and lauric acids), display the greatest antimicrobial activity, with lauric acid and its monoglyceride—monolaurin—having the strongest overall effect. Medium chain triglycerides are important components of mother’s milk. Medium chain fatty acids (MCFAs) also stimulate the production of white blood cells, boosting immune function. These and other fatty acids are essential in establishing the infant’s gut microbiome and provide protection from systemic infections.
Adults also benefit in a similar manner from the antimicrobial properties of fatty acids through the consumption of fats and oils. After weaning, we no longer enjoy the benefits of mother’s milk and the MCFAs it contains, but we can get MCAs through the consumption of dairy, as all mammal milks contain these protective fats. Other than dairy, there are only a few good dietary sources for MCFAs. The best natural sources are coconut and palm kernel oils. Coconut oil is by far the richest natural source, with even more than that found in mother’s milk. Coconut oil is composed of 63 percent MCFAs, with lauric acid comprising almost 50 percent. Palm kernel oil contains 53 percent MCFAs, with lauric acid making up about 45 percent. In comparison, butter, which is the third richest source, contains only 8 percent MCFAs. Most of the other fatty acids (long, medium, and short) possess varying degrees of antimicrobial fighting power and when consumed together, work synergistically to help protect us from infection.
Germs are everywhere. No matter how hard you try to scrub your dishes, clean your hands, and wash your food, germs are always present. Acids in our stomach kill most germs, but some manage to slip by to disrupt the gut microbiome or cause illness. The fats in our foods act as a secondary means of protection. In the digestive tract they destroy disease-causing organisms on contact. Fatty acids in the bloodstream help fight off systemic infections.
Unlike antibiotics, which kill only bacteria, fatty acids are effective against bacteria as well as viruses, fungi, and some parasites. For generations mothers have given their families homemade chicken soup to fight off the cold or flu (viral infections). As it turns out, a handful of scientific studies show that chicken soup really could have medicinal value.[2-4] Although these studies do not identify the exact ingredient or ingredients in the soup that make them effective, it might possibly be the fat. Homemade chicken soup is generally a rich source of fat.
So, when you eat a meal containing fat, you are eating food that will protect you from many forms of food poisoning and infectious disease. If, on the other hand, you avoid fat and eat low-fat foods, you are making it easier for germs to survive in your digestive tract and cause trouble. A healthy diet always includes ample amounts of fat.
HDL Cholesterol Protects Against Toxins
Saturated fats, and particularly lauric acid, increase the production of HDL cholesterol.[5-6] This is important because HDL has been shown to help protect against cardiovascular disease, reduce inflammation, and aid the immune system in fighting infections. HDL plays an important role in our defense by absorbing toxins produced by bacteria and transporting them to the liver where they are neutralized and excreted from the body.[7-8] Much of the harm caused by bacterial infections comes from the deleterious effects of bacterial endotoxins. HDL mops up these toxins and clears them from the body. Both animal and human studies have shown that higher HDL levels increase resistance to and reduce the risk of death from bacterial infections.[9-10] HDL is not only protective against bacteria, but has also been shown to inhibit the ability of certain viruses to penetrate our cells and to play an important role in defending against parasitic infections. Eating saturated fat or a low-carb diet have both been shown to be the most effective ways to increase HDL levels.
LPS Activate an Immune Response
The antimicrobial properties of dietary fats help train our immune system during infancy and keep it in good working order throughout life.
When we eat a meal, protein is broken down into amino acids and fat is broken down into fatty acids, making them small enough to penetrate the intestinal wall. Inside the intestinal wall, fatty acids and amino acids are combined into little bundles of fat and protein called chylomicrons. These chylomicrons travel from the lymphatic system to the bloodstream, where they circulate throughout the body delivering fat and protein to wherever they are needed.
As triglycerides are broken down in the gastrointestinal tract, fatty acids are released. Certain saturated and unsaturated fatty acids kill potentially troublesome bacteria. Many of the bacteria that are destroyed have an outer cell membrane composed of lipopolysaccharides (LPS). Some LPS fragments from the destroyed bacteria are small enough to pass through the epithelial lining and into the intestinal wall. Here the fragments are picked up with fatty acids, amino acids, and other substances and packaged into chylomicrons and are eventually carried into circulation.[11]
In the bloodstream, LPS is recognized as a foreign invader—a bacterium—and stimulates an immune response. Because of this process, some authors and researchers have suggested that eating high-fat diets promotes systemic inflammation leading to the development of obesity, diabetes, heart disease, and other disorders associated with chronic inflammation. They claim that dietary fat, particularly saturated fat, is inflammatory, and therefore causes chronic inflammatory related disease. In their zeal to find reasons to condemn dietary fat, the obvious is overlooked, as we shall see below.
Fat is an Important Part of a Healthy Diet
Fat has always been an important part of the human diet. Some populations, such as the Inuit, native Siberians, the Maasai of Africa, and many others subsisted and thrived on very high-fat diets. Over the past century thousands of people have adopted a very high-fat, ketogenic diet, some for extended periods lasting many years, and have not experienced obesity, diabetes, or heart disease. In fact, just the opposite happens; those on ketogenic diets generally lose excess weight, develop better blood sugar control, and reduce their risk of heart disease. The high-fat diet didn’t harm them, but made them healthier.
Fats are essential in establishing a healthy gut microbiome in newborn infants and in maintaining a healthy microbial population throughout life. The absorption of LPS is a normal and universal process that occurs in both humans and animals.[12] It is not a defect in biology or some freakish abnormality caused by eating fat. In animals, the process is the same. Carnivores and some omnivores, for example, eat a lot of meat and fat but do not become obese or develop diabetes or heart disease. However, dogs and cats fed pet foods high in processed grains, legumes, and other carbohydrates with only moderate fat, often do develop these human diseases. Obviously, meat and fat do not cause these problems in animals or in humans.
Fatty Acids Train the Immune System
In the body, when a white blood cell senses the presence of LPS, it interprets it as an invasion by potentially harmful bacteria and initiates an immune reaction by activating an inflammatory response and stimulating the production of more white blood cells and HDL cholesterol to defend the body. This is the body’s normal reaction to a potential threat. Contrary to popular belief, inflammation isn’t something that is bad or evil, it is the normal process in which the body mounts a defense and fights off infection. In most cases, it is a good thing, as it is protecting the body. Only when inflammation becomes chronic and never shuts down does it become a problem. This only happens when there is a stimulus that constantly triggers inflammation, such as chronic infection or tissue irritation. The slight inflammatory reaction from LPS after eating fat is usually only temporary and not a chronic condition even when fat is consumed at every meal. Interestingly, people who have been on very high-fat diets (60-80 percent of total calories consumed) for awhile generally have optimal C-reactive protein (CRP) levels. CRP is a marker for systemic inflammation. Those people who are diabetic, overweight, or at high risk for heart disease, have distinctively elevated CPR levels, indicating chronic inflammation.
While the consumption of some types of fatty acids do raise blood levels of LPS, markers for inflammation remain unchanged, indicating that high-fat meals do not trigger systemic inflammation, although there may be an increase in white blood cell production.[13] LPS can stimulate an inflammatory response, especially when it is associated with living bacteria, but apparently when the source of the LPS follows a fatty meal there is little or no accompanying inflammatory response. This is probably because LPS is from bacteria that are already dead and so there is no threat of an infection.
These LPS fragments trigger a mild immune response, which includes the increased production of white blood cells. White blood cells are the workhorse of our immune system and an increase in their numbers enhances immune function. More immune cells on the job means more cells are at work, seeking out and eliminating all potentially harmful troublemakers, not just bacteria, but viruses, yeasts, parasites, toxins, cancerous cells, and LPS fragments.
Instead of being a defect caused by a high-fat diet, the absorption of gut-derived LPS fragments is a normal and even necessary process of biology. LPS makes up the outer cell membrane of many pathogenic bacteria and is not the whole living organism. LPS is often used in medical research as a means to stimulate an immune response without the threat of causing an actual infection. Unlike living bacteria, it can’t multiply and grow. It is defenseless against the immune system.
For this reason, LPS provides a valuable tool to condition and train the immune system without danger. This is especially important in infants, whose immune systems are still developing and learning how to recognize harmful substances. Nursing infants eat a very high-fat diet. About 56 percent of the calorie content in human breast milk comes from fat, half of which is saturated fat. Many of these fats have the ability to kill potentially harmful bacteria in the gut. LPS fragments from the dead bacteria are then absorbed into the bloodstream and initiate a mild immune response. This way the infant’s immune system is trained to recognize harmful microorganisms. The slight increase in white blood cells boosts immune efficiency and the clearance of microbes and toxins from the bloodstream. This process continues in adults, keeping the immune system sharp and ready to leap into action whenever living invaders enter the bloodstream.[14]
LPS in large numbers, due to an active infection, can make you sick, but the small amount that enters the bloodstream from the digestive tract is too small to cause any noticeable symptoms or any harm. The release of LPS into the body from the gut is a normal, natural, harmless process. It couldn’t be otherwise, as this process occurs in all infants. Mother’s milk contains fats that kill potentially harmful bacteria in the gut. This releases LPS into the body. If this process was harmful, as some scientists have proposed, it would be very detrimental to newborn infants, whose immune systems are not yet completely functional. On the contrary, exposure to LPS helps train the infant’s immune system to recognize and mount a quick response to infection without the danger of an actual infection. This process is extremely important in developing our immune system as infants, and as adults it keeps our immune system in good working order. Dietary fats, and especially MCFAs, serve a very important role in training and maintaining proper immune function.
This article is adapted from Dr. Bruce Fife’s new book Fat Heals, Sugar Kills, published by Piccadilly Books, Ltd. 2019.
My new book Fat Heals, Sugar Kills describes why dietary fats are important to both your mental and overall health.
Available from Piccadilly Books, here
References
1. Miura, S, et al. Modulation of intestinal immune system by dietary fat intake; relevance to Crohn’s disease. J Gastroenterol Hepatol 1998;13:1183-1190.
2. Saketkhoo, K, et al. Effects of drinking hot water, cold water, and chicken soup on nasal mucus velocity and nasal airflow resistance. Chest 1978;74:408-410.
3. Hopkins, AB. Chicken soup cure may not be a myth. Nurse Pract 2003:28:16.
4. Rennard, BO, et al. Chicken soup inhibits neutrophil chemotaxis in vitro. Chest 2000;118:1150-1157.
5. Khaw, KT, et al. Randomised trial of coconut oil, olive oil or butter on blood lipids and other cardiovascular risk factors in healthy men and women. BMJ Open 2018;8:e0290167.
6. Hayek, T, et al. Dietary fat increases high density lipoprotein (HDL) levels both by increasing the transport rates and decreasing the fractional catabolic rates of HDL cholesterol ester and apolipoprotein (Apo) A-I. Presentation of a new animal model and mechanistic studies in human Apo A-I transgenic and control mice. J Clin Invest 1993;91:1665-1671.
7. Barbee, JF, et al. Apolipoproteins modulate the inflammatory response to lipopolysaccharide. J Endotoxin 2005:11:97-103.
8. Level, JH, et al. The protective effect of serum lipoproteins against bacterial lipopolysaccharide. Eur Heart J 1993;14:125-129.
9. Guo, L, et al. High density lipoprotein protects against polymicrobe-induced sepsis in mice. J Biol Chem 2013;288:17947-17953.
10. Iribarren, C, et al. Cohort study of serum total cholesterol and in-hospital incidence of infectious diseases. Epidemiol Infect 1998;121:335-347.
11. Ghoshal, S, et al. Chylomicrons promote intestinal absorption of lipopolysaccharides. J Lipid Res 2009;50:90-97.
12. Ravin, HA, et al. On the absorption of bacterial endotoxin from the gastro-intestinal tract of the normal and shocked animal. J Exp Med 1960;112:783-792.
13. Lyte, JM, et al. Postprandial serum endotoxin in healthy humans is modulated by dietary fat in a randomized, controlled, cross-over study. Lipids Health Dis 2016;15:186.
14. Nadhazi, Z, et al. Plasma endotoxin level of healthy donors. Acta Microbial Immunol Hung 2002;49:151-157.
The medium chain fatty acids (MCFAs) in coconut oil—lauric, capric, and caprylic acids—possess potent antimicrobial activity capable of killing disease-causing bacteria, viruses, and fungi. Although these fatty acids are deadly to potentially harmful microorganisms, they are harmless to friendly ones that are important for good digestive function and health. This is a good thing because another dietary source of these disease-fighting fatty acids is mother’s milk.
The digestive tract of a newborn is believed to be sterile. Exposure to the microorganisms from the mother’s birth canal, the hospital, the home, siblings, and elsewhere, quickly exposes the infant to a wide variety of microbes. However, the types of microbes that are established in the infant’s digestive tract are not left up to chance, but carefully controlled to produce the right proportions of the different organisms necessary for healthy digestive function. The MCFAs in mother’s milk are essential in this process. They suppress potential troublemakers and encourage the proliferation of good microbes, thus establishing a healthy gut microbiome.
The digestive tract begins at the mouth. Like the rest of the digestive tract, the mouth is populated by millions of bacteria and other microbes. One of the common inhabitants is Enterococcus faecalis. This bacterium is found to some extent throughout the digestive tract. In healthy people, the numbers of E. faecalis are kept relatively low and cause little problem. However, if its population grows too large or spreads to other parts of the body, it can cause life-threatening illness. According to the Centers for Disease Control and Prevention (CDC), E. faecalis is responsible for approximately 80 percent of cases of human infection.
This bacterium can cause infection when it enters wounds, blood, or urine. Hospital patients are particularly vulnerable because their immune systems are often compromised due to illness and because medical equipment, such as urinary catheter devices, are often contaminated with the bacterium. E. faecalis is believed to be one of the leading causes of hospital-acquired infections. It is a common cause of urinary tract infections, blood poisoning, infected wounds, endocarditis (infection of the heart), and oral infections—particularly those associated with root canals.
When a root canal procedure is performed, the dentist drills out the center of the dead tooth and then flushes it with a disinfectant to kill all the bacteria inside the tooth. The tooth is then packed with a filler to give it strength and prevent further infection. However, teeth are not solid blocks of calcium, but porous. Root canalled teeth become reinfected almost immediately. Teeth are specialized bones made up of living cells. They have blood vessels and nerves like other tissues. A root canalled tooth is dead. It no longer has access to the healing function of the immune system. In the mouth, it is in constant contact with millions of bacteria, including E. Faecalis, which migrate into the pores of the tooth. Here bacteria of all types can grow and thrive without threat from the immune system. Root canalled teeth become breeding grounds for bacteria which seep into the mouth and into the bloodstream taxing the immune system and causing chronic inflammation. Over time the constant release of bacteria into the body can contribute to a multitude of health problems including heart disease, diabetes, and arthritis.
E. faecalis is found to some extent in most people’s mouths but a poor diet and the presence of crowns, root canals, and periodontal disease can greatly increase their numbers. The process of oil pulling can greatly reduce the numbers of E. faecalis and other troublesome microbes. Oil pulling is simply swishing a spoonful of oil in the mouth like a mouthwash and spiting it out. The oil attaches to the bacteria and traps it during the swishing process. When the oil is spit out, the bacteria goes with it.
Any oil can be used for oil pulling, but coconut oil is the most effective. One of the reasons why coconut oil is better than others is because it contains antimicrobial medium chain fatty acids that not only pull out the bacteria but can kill it as well. When coconut oil is exposed to fat-digesting enzymes in saliva the medium chain fatty acids are released. The longer the oil is in contact with these enzymes the more MCFAs are produced. This is one of the reasons why it is often recommended that you oil pull for 15 to 20 minutes at a time, to take full advantage of the antimicrobial action of these fatty acids.
Numerous studies have shown the MCFAs can kill a variety of bacteria, viruses, and fungi, including oral bacteria such as Streptococcus mutans—a common cause of tooth decay. [1] These fatty acids are also effective against E. faecalis.
E. faecalis is the most commonly implicated infectious organism associated with root canals. The most widely used solution to disinfect root canalled teeth is sodium hypochlorite (NaOCl). It is a potent antimicrobial agent and effectively dissolves pulpal remnants when used in concentrations ranging from 0.5 to 5.25 percent. However, NaOCl has an unpleasant taste and has been criticized for its relative toxicity.
Researchers at Kannur Dental College, Kannur, India investigated the antimicrobial potency of MCFAs in comparison to NaOCl and two other disinfectants—chlorhexidine gluconate and ethanol. A 2 percent chlorhexidine solution is used as a potent antibacterial mouthwash for the treatment of gingivitis. It is a prescription drug that can cause tooth staining, mouth irritation, decreased taste sensation, and tongue swelling. Ethanol, also known a grain alcohol, is used as an antiseptic and disinfectant. It is commonly used in antibacterial hand sanitizers and medical wipes.
The researchers compared the antimicrobial efficacy of lauric, capric, and caprylic acids against E. faecalis to 5 percent NaOCl, 2 percent chlorhexidine, and ethanol. The test was conducted using an agar filled Petri dish.
E. faecalis was chosen for the study because it is resistant to many disinfecting agents and is a common cause of oral infection. It can survive harsh environments such as extreme alkaline pH, salt concentrations, temperature of 60 degrees C (140 F), and resists degrading by bile salts, detergents, heavy metals, azide, and desiccation. NaOCl and chlorhexidine are some of the few antibacterial agents that are effective against E. faecalis.
Using a Petri dish filled with agar, six dimples were made in the agar with each one filled with a measured amount of one the six test substances. The agar was exposed to E. Faecalis and incubated for 24 hours. During this time, the bacterium grew over the agar except at the locations containing the test substances. The antibacterial strength of each test substance was determined by measuring the diameter of the dead zone formed around each one.
All of the MCFAs demonstrated significant antimicrobial activity against E. Faecalis, with lauric acid showing the greatest effect. The 2 percent chlorhexidine solution showed the greatest overall effect with a dead zone extending out for 21.6 mm, followed by lauric acid (17.66 mm), 5 percent NaOCl (16.33 mm), capric acid (14.00 mm), caprylic acid (12.33 mm), and finally ethanol (9.67 mm). [2]
The antimicrobial action of the MCFAs were comparable to that of 5 percent NaOCl, with lauric acid a little stronger and capric and caprylic acids a little weaker. The advantage of MCFAs is that they are nontoxic to humans and have no adverse side effects, giving them a clear advantage over NaOCl.
Many substances have a synergistic effect, in that when they are combined, they have a greater effect than each on their own. It is quite possible that the combination of all three MCFAs has such a synergistic effect that may give them the potency comparable to 2 percent chlorhexidine solution.[3] Oil pulling has proven effective in reducing S. mutans and other oral bacteria, producing results superior to antimicrobial mouthwashes, without the undesirable side effects.[4-5]
Coconut oil can not only protect your teeth and gums from E. faecalis through oil pulling, but when ingested can help clear this troublesome bacterium from your digestive tract as well. Virtually everyone who has a root canalled tooth has an overgrowth of E. faecalis, and probably numerous other unsavory bacteria, in their mouths and probably the rest of their bodies. Consuming coconut oil regularly and oil pulling daily can be an effective way to reduce the bacteria populations in your mouth, reduce the risk of spreading oral bacteria through your bloodstream, and keep your gut microbiome in balance.

Antibacterial strength is determined by measuring the dead zone around the test substances in a Petri dish.
References
1. Nordqvist, C. Coconut oil may prevent tooth decay. Medical News Today Sep 4, 2012.
2. Devan, K, et al. Antimicrobial efficacy of medium-chain fatty acids, 2% chlorhexidine, and 5% sodium hypochlorite against Enterococcus faecalis: An in vitro study. Indian J Oral Health Res 2018;4:47-51.
3. The effect of coconut oil pulling on Streptococcus mutans count in saliva in comparison with chlorhexidine mouthwash. J Contemp Dent Pract 2016;17:38-41.
4. Asokan, S, et al. Effect of oil pulling on Streptococcus mutans count in plaque and saliva using Dentocult SM Strip mutans test: a randomized, controlled, triple-blind study. J Indian Soc Pedod Prev Dent 2008;26:12-17.
5. Shino, B, et al. Comparison of antimicrobial activity of chlorhexidine, coconut oil, probiotics, and ketoconazole on Candida albicans isolated in children with early childhood caries: an in vitro study. Scientifica 2016, Aricle ID 7061587, 5 pages.
If you look at the ingredients in foods today, it seems that canola oil is found in the vast majority of them—both conventional foods and so-called health foods. In addition, restaurants often use canola oil for deep frying and you can purchase it to use for meal preparation at home. Unless you are very careful it is almost impossible to avoid consuming canola oil.
With the realization that hydrogenated vegetable oils are unhealthy and pronouncement by the FDA that they should be eliminated from our diet, food manufacturers and restaurants have looked for suitable replacements–oils that are shelf stable and resistant to temperatures used in food preparation. The most suitable fats for this purpose are saturated fats like coconut oil, palm oil, and beef tallow. However, the lingering fear of saturated fats has prevented the complete acceptance of these types of fats back into the diet. For this reason canola oil, which is composed primarily a monounsaturated fat, has been a popular choice to replace hydrogenated vegetable oils in cooking and frying. Although monounsaturated fats are not as tolerant to heat as saturated fats are, they are more stable than polyunsaturated fats.
Canola oil is often promoted as a healthier alternative to saturated fats and hydrogenated vegetable oils. A new study, however, suggests that it may just as harmful as the latter.
One of the primary drawbacks to canola oil is that the vast majority of it is produced from genetically engineered rapeseed plants that are designed to survive exposure to repeated heavy doses of pesticides. Invariably, this intense exposure of pesticides leaves a residue when the seeds are processed into oil. Both pesticides and genetically modified organisms (GMOs) have been linked to various health problems ranging from cancer to birth defects and infertility.
The study suggests that canola oil can cause brain damage and promote weight gain. Whether this effect is caused by the pesticide residue, the altered genetic makeup of the canola plant, or the formation of harmful byproducts resulting from high-heat processing and cooking is not clear.

The study involved two groups of mice, one group was given a regular diet, and the other was given the same diet along with a supplement of canola oil. After 6 months the mice were subjected to a number of tests. The mice that had received the canola oil showed memory deterioration and degenerative learning ability. An examination of the brains showed an increased amount of plaque commonly associated with Alzheimer’s disease. Additionally, the canola oil fed mice gained considerably more weight than those with no canola oil in their diet. [1]
Based on this study, it appears that if you want to significantly increase your risk of Alzheimer’s disease and obesity, consuming canola oil would be a good way to accomplish this. In contrast, coconut oil has been shown to reverse the effects of Alzheimer’s and improve memory [2, 3] as well as promote weight loss [4]. Coconut oil also is far safer to use in food preparation as it is more resistant to degradation and free-radical formation during cooking. [5] Unlike canola oil, coconut oil is not genetically engineered and rarely exposed to pesticides, making it a far better choice for health-conscious individuals.
References
1. Lauretti, E. and Pratico, D. Effect of canola oil consumption on memory, synapse and neuropathyology in the triple transgenic mouse model of Alzheimer’s disease. Scientific Reports 17134 (2017).
2. Nafar, F, et al. Coconut oil protects cortical neurons from amyloid beta toxicity by enhancing signaling of cell survival pathways. Neurochem Int 2017; 105:64-79.
3. Rahim, NS, et al. Enhanced memory in Wistar rats by virgin coconut oil is associated with increased cholinergic activities and reduced oxidative stress. Pharm Biol 2017;55(1):825-832.
4. Liau, KM, et al. An open-label pilot study to assess the efficacy and safety of virgin coconut oil in reducing visceral adiposity. ISRN Pharmacol 2011:949686.
5. Srivastava, Y and Semwal, AD. A study on monitoring of frying performance and oxidative stability of virgin coconut oil (VCO) during continuous/prolonged deep fat frying process using chemical and FTIR spectroscopy. J Food Sci Technol 2015;52:984-991.
Stop Alzheimer's Now!
How to Prevent and Reverse Dementia, Parkinson's, ALS, Multiple Sclerosis, and Other Neurodegenerative Disorders
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
For a description or to order click here
We have it drilled into us that high cholesterol is bad, especially our LDL or “bad” cholesterol. Too much cholesterol, we are told, increases our risk of heart attack and stroke. For this reason, many people assume that the lower they can get their cholesterol, the better. But low cholesterol may be just as bad as or even more harmful than high levels.
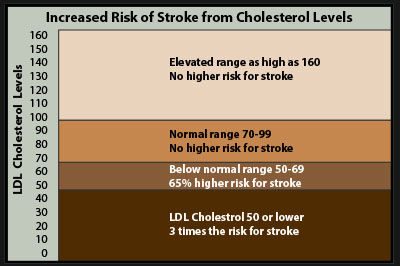
A study headed by researchers from Pennsylvania State University discovered that low LDL cholesterol levels increase your risk of suffering a hemorrhagic stroke, the type which is caused by the rupture of a blood vessel in the brain. About 13 percent of all strokes are of the hemorrhagic type.
The researchers studied 96,043 people for an average of nine years, recording their LDL levels biennially and tracking cases of hemorrhagic stroke. The normal range for LDL is 70 to 99 mg/dl. The researchers found that people who had an LDL of 50 to 69 mg/dl had a 65 percent higher risk of hemorrhagic stroke. For people with an LDL below 50, the risk nearly tripled.
LDL levels above 100 mg/dl, generally considered to be undesirable, were not associated with hemorrhagic stroke, even at levels higher than 160.[1]
Although LDL cholesterol is commonly referred to as the “bad” cholesterol, it isn’t inherently bad in itself. It only becomes bad or harmful if it is damaged by oxidation. Otherwise, LDL cholesterol is beneficial. It is the type of cholesterol that the body uses to make hormones such as testosterone and estrogen, as well as vitamin D and bile, and constitutes an important structural component of cell membranes and nerve tissue. It is essential for the proper brain function. The brain contains the highest concentration of cholesterol in our bodies.[2] Low cholesterol has been associated with an increased risk of Alzheimer’s disease, psychiatric disorders, and cognitive impairment.[3-5] It is really no surprise that a lack or a deficiency of cholesterol would increase the risk of hemorrhagic stroke.
References
1. Chaoran, M, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage A prospective study. Neurology 2019; doi: 10.1212/WNL.0000000000007853.
2. Bjorkhem, I. and Meaney, S. Brain cholesterol: Long secret life behind a barrier. Arteriosclerosis Thrombosis and Vascular Biology 2004;24:806-815.
3. Mason, R.P., et al. Evidence for changes in the Alzheimer’s disease brain cortical membrane structure mediated by cholesterol. Neurobiol Aging 1992;13:413-419.
4. Elias, P.K., et al. Serum cholesterol and cognitive performance in the Framingham Heart Study. Psychosom Med 2005;67:24-30.
5. Conklin SM and Stanford MS. Premeditated aggression is associated with serum cholesterol in abstinent drug and alcohol dependent men. Psychiatry Res 2008;157:283–7.
Superfoods are known for their extraordinary health and healing properties. Among all the superfoods, there is one that stands head and shoulders above the rest, and that is coconut, and more specifically, coconut oil.
Coconut oil contains the highest natural source of medium chain fatty acids—a unique type of fat with remarkable health-promoting properties. These special fatty acids are crucial for achieving optimal health and make coconut oil not just a health food, but a super health food.
Some superfoods get their reputation because they have anti-cancer properties or can stabilize blood sugar. Others have been shown to reduce the risk of heart disease or Alzheimer’s or improve digestive function and protect against inflammatory conditions such as arthritis or inflammatory bowel disease. Coconut oil can do all these things plus much, much more.
In fact, coconut oil can do more for your health than the next ten leading superfoods combined. For this reason, it can rightfully claim the title as the world’s most powerful superfood. This isn’t an empty claim. This is what the science shows. All of the health-promoting properties of coconut oil described in this book are documented by published medical research. Once you see the evidence yourself, you will agree that coconut oil is nature’s premier superfood.
This book is available free of charge on Amazon as a Kindle eBook. Go here to download the book. No cost or obligation.
Top of Page
Body Electric Summit: October 7-13, 2019
Your body is more than a set of biochemical interactions. It is time to see your body as ENERGY. Join us and learn precisely how you can ACCESS that energy, as part of your health journey and get the tools and learn the language of your “Body Electric!”
Essential Oils Transformation: October 14-20, 2019
With all the fear, hype and confusion surrounding essential oils it can be nearly impossible to find a straight answer about safety, benefits and usage. But essential oils don’t need to be complicated! Anyone can learn how to use these powerful and approachable tools to enhance their lives and invite more natural solutions into their homes.
Lupus and Autoimmunity Summit: October 21-27, 2019
Millions of people worldwide suffer needlessly with the symptoms of systemic lupus erythematosus. Conventional medical treatment for this mysterious disease is limited to symptom management and doesn’t address the underlying reasons for why the person developed this devastating, life altering condition, or do anything to actually fix the problem. But, it doesn’t have to be this way. Find answers at this summit.
Get Off Your Sugar Summit: November 4-10, 2019
Do you need help breaking the sugar habit? This summit is designed for you. Get the help you need from the experts.
Issue 16-3 covers: Does Low Cholesterol Cause Alzheimer’s?—Keto Cycling: How to Optimize the Ketogenic Diet and Avoid Common Mistakes—Consumer Alert! Do You Know Where Your Foods and Supplements Come From?—Why Scientists Are Opposing 5G Networks